Pharmacy First and patient care records
Integration of community pharmacy with other primary care professionals through technology has been a goal for both pharmacists and the NHS for many years.
Pharmacy First (PF) has brought together and updated the technology available to community pharmacies in England to enable greater integration into primary care. It has speeded up the adoption of electronic communication with both patients and GP practices. Similar systems are in use or being introduced across the UK.
With the patient’s consent, their GP record via GP Connect, the NHS care record or an alternative clinical record must be checked by the pharmacist unless there is good reason not to do so. Access to the care record can also help ascertain whether the patient may have a diagnosed condition listed in a PGD or PF pathway as excluding that patient from treatment. This overcomes the problem of a patient not knowing or remembering specific diagnoses.
Pharmacists must adhere to defined standards of record keeping, ensuring that the consultation record is made on the same day that it occurs unless exceptional circumstances apply. The details and outcome of each consultation should be recorded. For PF purposes, this record should be made on the Pharmacy First IT system (PFIT). Where PFIT is unavailable due to exceptional circumstances, the record of the consultation must be added to the system as soon as possible after it becomes available again.
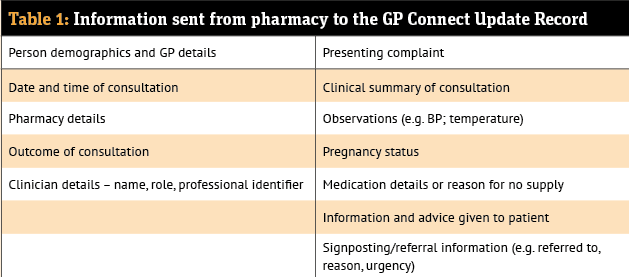
Pharmacy contractors must ensure that a notification of the provision of a PF consultation is sent to the patient’s general practice on the day of provision, or on the following working day. Where possible, this should be sent as a structured message in real-time using the PFIT.
In the absence of an automated digital solution, or if there is a temporary problem with the system, the information should be sent via NHS mail or hard copy.
GP Connect
GP Connect provides the functionality to automatically update a patient’s GP medical record. Where an action is required by the general practice team, such as booking the patient in for follow-up or an appointment, an ‘action message’ or ‘urgent action communication’ must be sent to the practice.
Tips for completing the record include:
- Record directly onto the software system and do not use paper/pen unless it is unavoidable
- Consider what is written from the point of view of another health professional or the patient who might read it
- Include relevant social history
- It is important to record negative as well as positive findings to show that all aspects have been considered
- For fields that are not applicable, write “N/A” rather than leave blank. This shows that the item has been considered and was not missed.
NHS England advises: “Pharmacy teams should work on the basis that when a consultation record is submitted, the information shared will be available to GPs, other health and care providers, and patients (and their proxy users) via patient facing services. Consequently, clinical records should not include any information that can not be viewed via patient facing services or by clinicians in other care settings.”
A ‘proxy user’ is defined as a family member, medical next of kin, a close friend or carer, whom a patient would usually trust to act on their behalf.
Pharmacists will sometimes want to send information from the consultation to a GP practice via NHSmail – for example, where there is a safeguarding concern or another reason why the patient may not want details of their consultation visible via patient facing services (e.g. so they may be seen by a friend or relative who has been given access as a proxy user).
When providing the Pharmacy Contraception Service, for instance, there may be a safeguarding concern or other reason why a patient might not want their consultation details visible via patient facing services or the Summary Care Record (e.g. a person under 16 years of age who is receiving contraception services and may not want others to see this information). In these cases, pharmacists should capture in the consultation record that the patient does not consent to their information being shared with the GP.