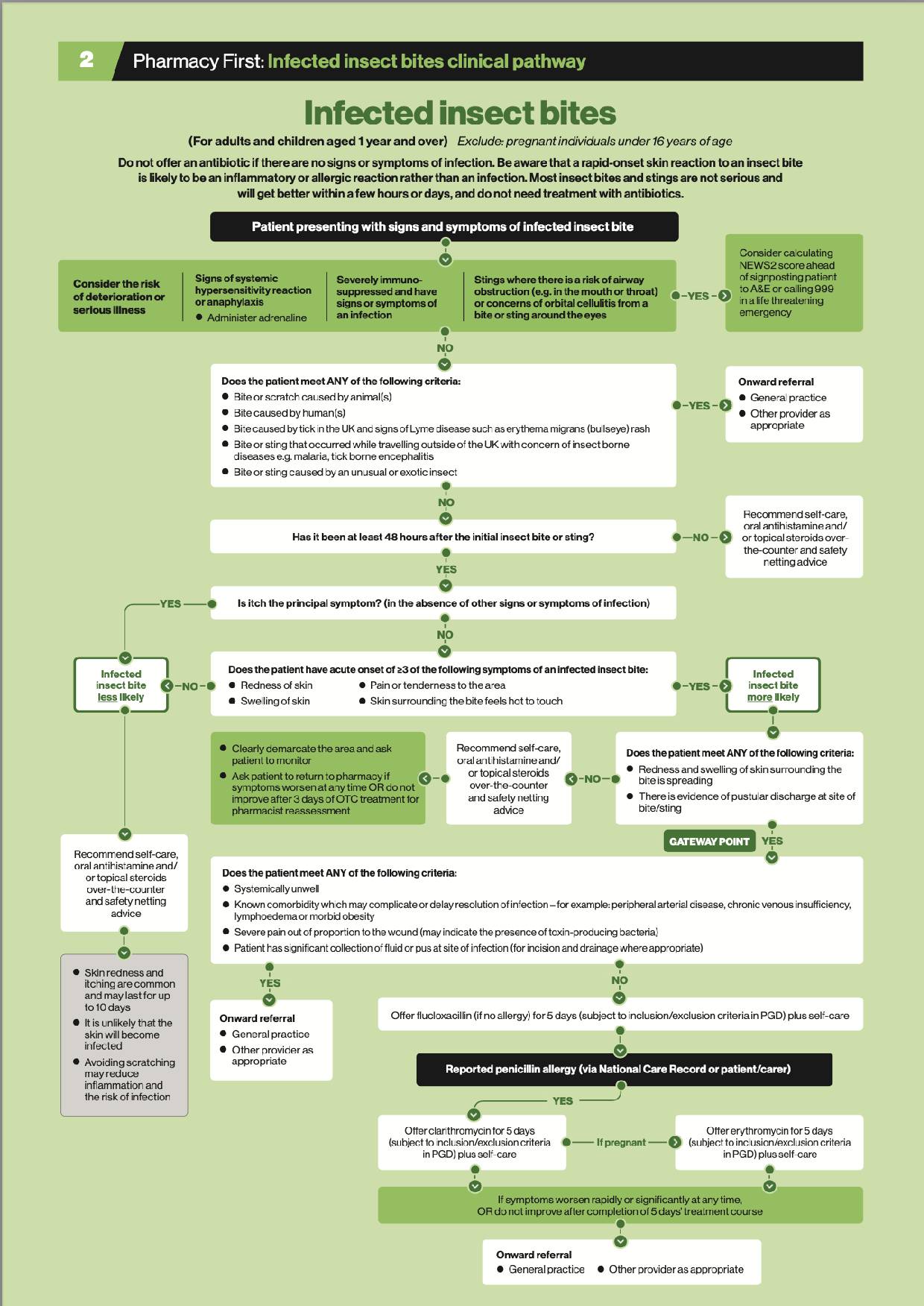
Clinical pathway
Download a PDF of the clinical pathway here.
When to treat
Insect bites and stings tend to be a seasonal phenomenon and mostly occur in rural areas. Most are uncomplicated and will heal spontaneously. They may be intensely itchy and inflamed for a few days, so patients may need reassurance and first aid measures and require some symptomatic treatment.
However, inflamed and often excoriated skin presents an opportunity for infection and a small number of insect bites or stings will become infected a few days after the initial injury. These require treatment to prevent the development of more serious conditions such as cellulitis or sepsis.
There is no need for prophylactic antibiotic treatment of insect bites and stings. Rapid-onset reactions to bites or stings are more likely to be allergic or inflammatory in nature rather than an infection.
People can be bitten by insects (which have six legs) such as mosquitoes, midges and horseflies, and by arachnids (which have eight legs) such as mites and ticks. In this toolkit, the term ‘insect’ is used for both groups.
Some insects (such as mosquitoes, bed bugs and fleas) have piercing mouth parts that cause little trauma and may not be noticed immediately. Others (such as horseflies and midges) lacerate the skin and lap up blood from the wound. Such bites are painful and are noticed immediately.
Stinging insects include bumble bees, honeybees, wasps and hornets. They inject venom, which contains a mixture of pharmacologically active substances (e.g. allergens, histamine). The sting is usually felt immediately. Honeybees have a barbed stinger and venom sac, which is left in the skin as the insect flies away.
Taking a history
Ask about the onset, site, appearance and duration of symptoms including:
- Local symptoms such as pain, swelling and erythema
- Symptoms that could indicate a systemic reaction such as urticaria, rhinitis, wheezing, abdominal pain, vomiting and dizziness
- Risk factors for insect bites or stings such as outdoor activities, contact with domestic pets, overseas travel or contact with infested individuals (scabies)
- Was the bite or sting witnessed as being inflicted by a specific insect?
- Has there been a history of serious reactions to insect bites or stings in the past?
- Have any over-the-counter or prescribed preparations been used? In some people, topical preparations can cause allergic or sensitivity reactions.

There is no need for prophylactic antibiotic treatment of insect bites and stings. Rapid-onset reactions are more likely to be allergic or inflammatory in nature
The appearance of bites and stings varies. Many will start as a small red mark or papule. Sometimes there is inflammation or swelling around the initial bite or sting and this may develop over several days.
Occasionally, insect stings can cause large local reactions (LLR), with inflammation spreading over an area greater than 10cm within 24 to 48 hours, and resolving in three to 10 days.
The prime purpose of the examination is to look for the clinical features of an infected insect bite or sting. Use the clinical pathway for infected insect bites and stings (above) to guide your diagnosis.
Patients who have bites inflicted by animals, unusual insects or while travelling abroad where there is a risk of malaria or tick-borne encephalitis, may require onward referral to their GP. This may also be the case if the bite as caused by a tick in the UK and the patient is showing signs of Lyme disease such as erythema migrans (bullseye) rash.
However, if the bite occurred over 48 hours previously and the patient is showing three or more of the following symptoms, an infected insect bite is more likely:
- Redness of the skin (erythema may be more difficult to distinguish on darker skin tones)
- Pain or tenderness to the area
- Swelling of the skin
- Skin surrounding the bite(s) feels hot to touch.
If, in addition, the redness and swelling of the skin surrounding the bite is spreading, or there is evidence of pustular discharge at the site of the bite/sting, then the Gateway Point has been reached.
If these criteria are not met, then recommend self-care and ask the patient to return to the pharmacy for re-assessment if symptoms worsen or do not improve after three days of OTC treatment.