Treatment options
Practical advice
Practical advice for managing shingles is to wear loose-fitting clothes to reduce irritation and to cover lesions that are not under clothes with a non-sticky dressing while the rash is still weeping.
Patients should be advised to avoid work, school or day care if the rash is weeping and cannot be covered.
Since people could catch chickenpox from someone with shingles if they have not had it before, patients should try to avoid:
- Anyone who is pregnant and has not had
chickenpox before - People with a weakened immune system
- Babies less than one month old.
If the lesions have dried or the rash is covered, avoidance of these is not necessary.
Topical creams and adhesive dressings should generally be avoided as they can cause irritation and delay rash healing.
Other advice includes:
- Keeping the sores clean and dry, but not using scented soaps or bath oils and not rubbing too hard as this will delay healing
- Not letting dressings or plasters stick to the rash
- Applying ice cubes in a plastic bag wrapped in a tea towel. A pack of frozen peas wrapped in a tea towel or a gel ice pack may also help.
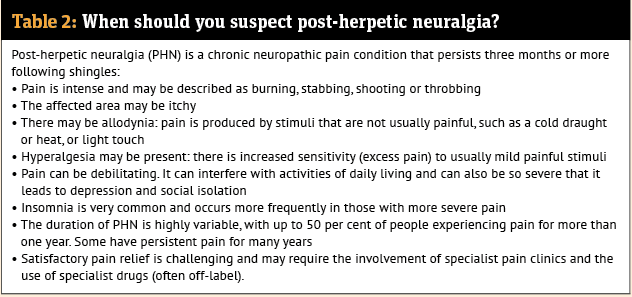
Pain
The pain from shingles has been found to range from mild to severe. Adults with mild pain can try paracetamol alone or in combination with codeine or ibuprofen. If this does not work, or the person presents with, or develops, severe pain, referral is indicated. Prescribers may offer a trial of treatment intended for neuropathic pain, usually amitriptyline (off-label use), duloxetine (off-label use), gabapentin or pregabalin.
Antivirals
For early cases of shingles, a course of oral aciclovir or valaciclovir may be used. There is evidence that the earlier treatment is started within 72 hours of rash onset, the more it may reduce the severity and duration of a shingles episode.
Pharmacists are now able to initiate this early treatment. Community pharmacy PGDs, for example in Scotland, make more specific requirements for treatment initiation, usually relating to restricting it to within 72 hours of onset, to those with a single affected dermatome on the torso and in patients who are aged over 18 years.
In England, both the aciclovir and valaciclovir PGDs list patient inclusion criteria as a diagnosis of shingles within 72 hours of rash onset AND ANY of the following:
- Non-truncal involvement (e.g. shingles affecting the neck, limbs or perineum)
- Moderate or severe pain
- Moderate or severe rash (defined as confluent lesions)
- Aged over 50 years and/or immunosuppressed.
Also, those diagnosed with shingles within seven days of rash onset AND ANY of the following:
- Immunosuppressed (see Clinical Pathway)
- Continued vesicle formation
- Severe pain
- High risk of severe shingles (e.g. severe atopic dermatitis/eczema)
- Aged 70 years and over.