Examining the patient
Before any examination the patient’s (or parent’s) consent should be sought and, of course, hand washing is required. It is good practice to check for a raised temperature using a thermometer.
Younger children may not have a clear cause for being miserable and unwell other than symptoms and signs of a respiratory infection, so it may be necessary to do an overall assessment and examine the throat as well (see Sore Throat modules, PM January and February issues).
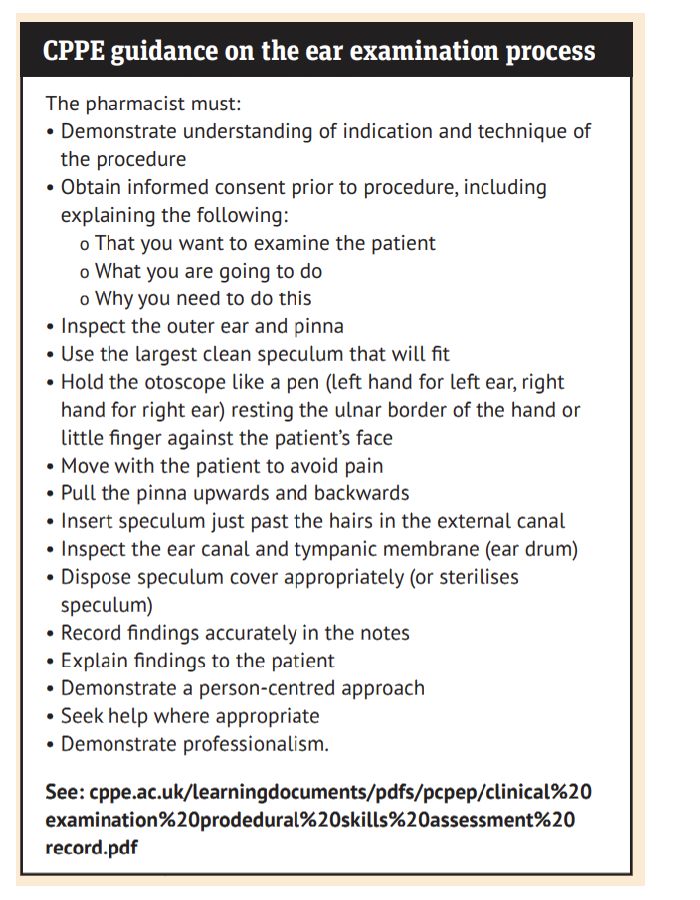
Learning to examine ears using an otoscope ideally requires supervised training. The more this is practised, the more competent pharmacists will become. A normal ear drum is translucent and greyish in colour. Practise on staff or family (with their consent) to get familiar with using an otoscope and understand what a normal ear drum looks like.
There are some useful training resources including a short video from BMJ Learning.
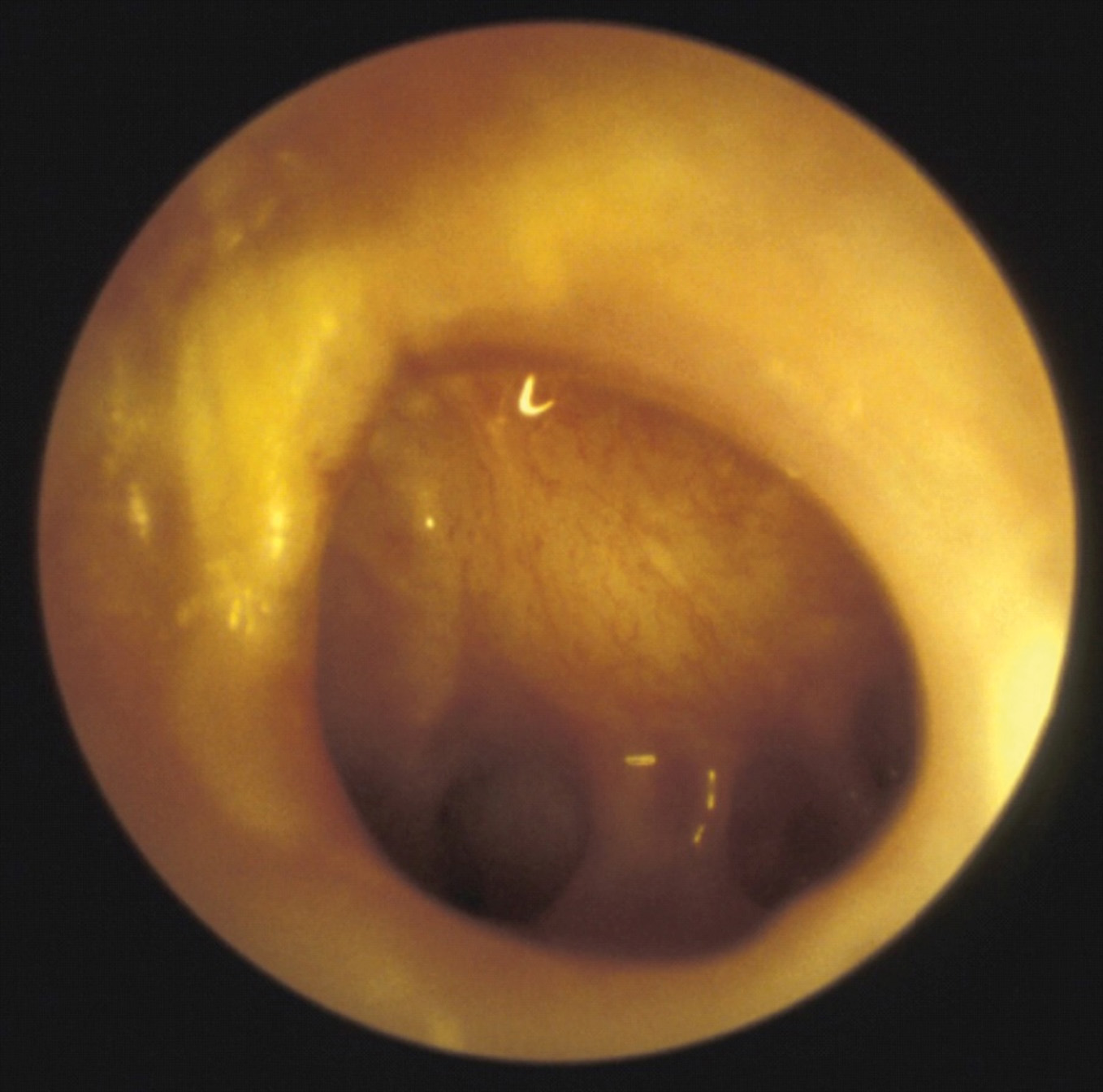
There is also a link to BMJ Learning – The tympanic membrane – diagnostic picture tests (you will need to register to access both. A list of competencies for ear examination is provided by CPPE (see below).
Examining children can be difficult, particularly if they are fractious or unwell and not co-operating. There are various techniques for reassuring the child and helping them to feel at ease.
Introduce the suggestion that the examination is fun, like play acting, especially in children over three years of age. The child may have play acted such activities using a toy doctor’s kit. Another tip is to ask if there is light coming out of the other ear. These small things can make a big difference.
The child should sit on an adult’s lap, held sideways for examining the ears. Both the child’s hands should be secured by the adult with one hand, the head held firmly against the chest with the other.
The otoscope should be held lightly, like a pencil between thumb, index and middle fingers. The little finger can be rested on the forehead, providing support and allowing movement with the head. This will need to be repeated with the head held the other way for the other ear.
Increasingly, fibre optic digital otoscopes are being used rather than the traditional optic lens-based devices. These connect to smart phones or tablets via Bluetooth or wi-fi, or are attached directly to the device, so the ear drum can be visualised on screen. They have a wide angle of view at the tip and are generally easier to use and less invasive.
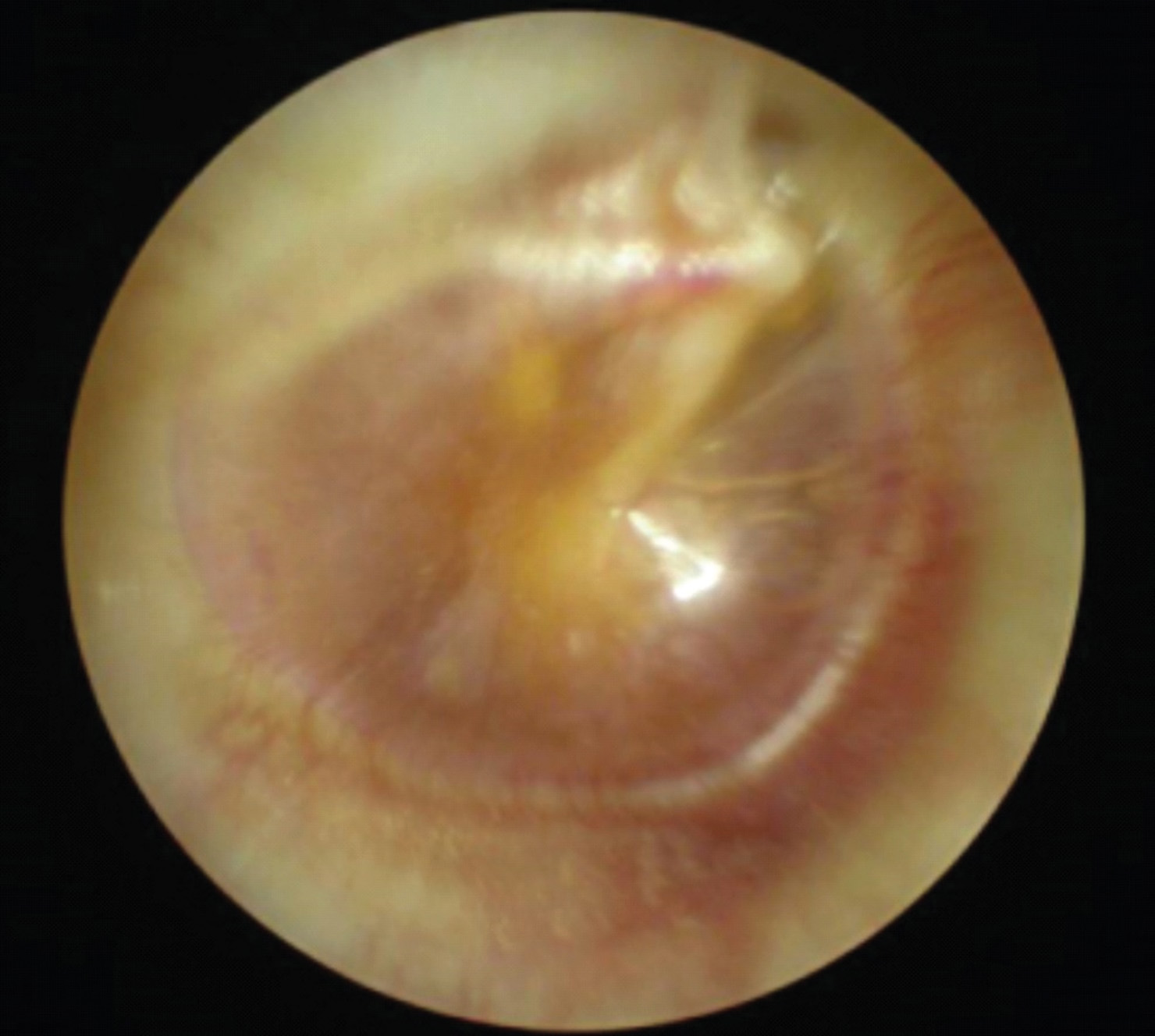
The main impediments to seeing the ear drum clearly are debris, inflammation of the ear canal (usually due to otitis externa) or wax, which appears as a yellowy, orange or brown deposit.
If the ear drum has perforated due to infection, there may be pus in the ear canal – usually yellow or green.
The main diagnostic features of acute otitis media, as advised by the patient group directions used in England’s Pharmacy First service, are:
- A distinctly red, yellow or cloudy tympanic membrane
- Moderate to severe bulging of the tympanic membrane, with loss of normal landmarks and an air-fluid level behind the tympanic membrane (indicates a middle ear effusion).
- Perforation of the tympanic membrane and/or discharge in the external auditory canal.