When to suspect acute sinusitis
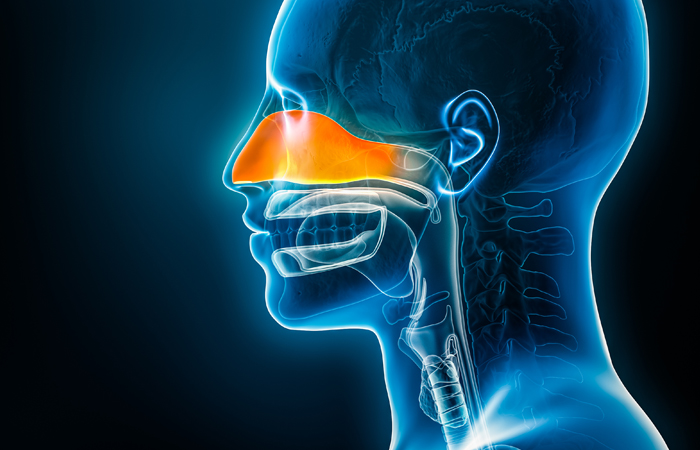
The paranasal sinuses are air-containing spaces in the bony structures adjacent to the nose (maxillary sinuses) and above the eyes (frontal sinuses). During a cold, their lining surfaces become inflamed and swollen, producing mucus. The maxillary sinuses are most commonly involved.
The secretions drain into the nasal cavity and, if the drainage passage becomes blocked, fluid builds up in the sinus. This causes pain from pressure – acute sinusitis. Rarely it can become secondarily (bacterially) infected. If this happens, more persistent pain arises in the sinus areas, and there may be fever and purulent nasal discharge.
The PGDs for supply of treatments for acute sinusitis under the Pharmacy First scheme use the following diagnostic criteria (derived from CKS):
- Presence of ONE of the following signs/symptoms which suggest acute sinusitis:
- Nasal blockage (obstruction/congestion) OR
- Nasal discharge (anterior/posterior nasal drip).
AND ONE or more of the following:
- Facial pain/pressure (or headache) OR
- Reduction (or loss) of the sense of smell (in adults) OR
- Cough during the day or at night (in children).
As noted, there may be a reduction or loss of the sense of smell. Other features suggestive of acute sinusitis are altered speech indicating nasal obstruction, and tenderness, swelling or redness over the cheekbone or periorbital areas. To diagnose sinusitis rather than the after-effects of a viral respiratory tract infection, symptoms should be present for 10 days or more with little improvement.