What medicines should be prescribed for HFrEF?
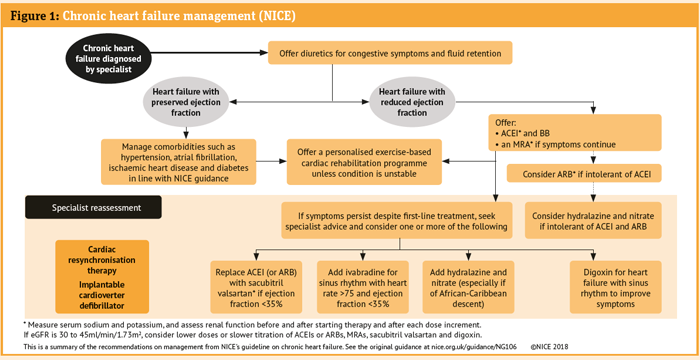
There is a substantial evidence base to support the use of medicines in HFrEF to reduce both mortality and morbidity and thus have a prognostic benefit in patient management. Figure 1 (below) shows the NICE guideline recommendations for HFrEF.
If there is congestion/fluid overload, a diuretic should be prescribed. This would usually be a loop diuretic such as furosemide or bumetanide with the dose titrated to the minimum required to control symptoms. Careful monitoring of renal function and electrolytes is important. The diuretic may be stopped, or the dose reduced, as the congestion resolves.
In resistant cases it is important to check patient adherence as diuretics can have significant effects on quality of life; patients may choose to omit doses if they are interfering with their daily activities or causing nocturnal symptoms.
However, where diuresis is difficult, management may involve adding a thiazide diuretic (e.g. bendroflumethiazide or metolazone) every day or perhaps on alternate days – often for a short period of time, under specialist review.
Due to differences in bioavailability it is important the correct metolazone product is selected. The licensed formulation Xaqua is preferred on clinical grounds to imported metolazone preparations for new patients or after careful switching of existing patients by specialist heart failure teams.
Assessment of symptoms and the use of ‘daily weights’ (morning weight after going to the bathroom and before eating or drinking) are helpful as a measure of fluid loss – patients should aim for a weight loss of no more than 0.5-1.0kg a day. Rapid diuresis may result in acute kidney injury. Electrolyte loss is also common.
Failure to respond to combinations of loop and thiazide diuretics, hyponatraemia, worsening renal impairment or ongoing weight gain (indicating further fluid retention) would warrant specialist input and may require admission to hospital, a day care unit or virtual ward – depending on the availability of local services – for intravenous diuretics.
Prognostic medications should also be introduced and doses optimised. The traditional approach to treatment was the introduction and titration to target/maximally tolerated doses of:
- An ACEI or alternatively an ARB if the patient experiences side-effects such as ACEI cough; or a beta-blocker licensed in the UK for heart failure (bisoprolol, carvedilol or nebivolol)
- Subsequent introduction of a MRA (spironolactone or eplerenone) in symptomatic patients.
Dose titration requires monitoring of blood pressure, renal function, potassium (risk of hyperkalaemia), sodium (risk of hyponatraemia) and heart rate/pulse. Although titration to the maximum/maximum tolerated doses is important to realise optimal patient outcomes, this does not always happen in practice.
A medication review is an effective way of identifying patients where suboptimal doses are prescribed and then referring patients to their GP or heart failure team, depending on local services, to ensure that their treatment is optimised.