Drug interactions with statins
There are some significant drug interactions with statins that may affect choice of therapy or limit the maximum dosage that can be prescribed.
Many, but not all, of the interactions are due to inhibition of the cytochrome P450 3A4 pathway. Simvastatin is the most affected in the class, but atorvastatin is often also affected. Interacting drugs include macrolide antibiotics, antifungal agents, medicines for HIV, calcium channel blockers, amiodarone, warfarin and ciclosporin.
This is not an exhaustive list and up-to-date information should be consulted, as well as consideration of potential interactions with herbal and OTC medicines.
Grapefruit/grapefruit juice also inhibits statin elimination so should be avoided when taking simvastatin and limited to no more than a small glass of juice per day in patients taking atorvastatin.
Adverse effects of statins
Some people who take statins experience muscle pain, cramps and/or weakness. Although data from clinical trials suggests that the numbers do not differ much between those patients allocated to active treatment or placebo, in clinical practice a significant minority of patients will complain of this side-effect.
It is most likely to occur in the first three to 12 months of treatment and may be more common in people with underlying comorbidities, such as renal impairment or untreated hypothyroidism. It is also more common with increasing age, Asian ethnicity, female gender, or as a result of drug interactions.
Typically, it affects the large muscle groups (shoulder, pelvic girdle, arms and legs) and is symmetrical in nature. Rarely, some people taking statins have developed rhabdomyolysis – abnormal muscle breakdown, which can lead to kidney problems and be life-threatening.
If a patient reports side-effects suggesting muscle problems with a statin, a blood test for creatine kinase (CK) should be undertaken. If there is only a mild increase in CK (less than four-five times the upper limit of normal) with tolerable symptoms, the patient can be reassured and, in most cases, the statin continued unchanged.
For more symptomatic patients or those with a larger rise in CK, alternative strategies will be needed, depending on severity of the symptoms, magnitude of the rise in CK and clinical urgency. More detailed guidance can be found in the national statin intolerance pathway.
Other adverse effects or cautions include:
- Liver toxicity: statins are contraindicated in active liver disease. Minor increases in liver enzymes (transaminases) are often seen in the first three months of statin therapy. Temporary discontinuation and further assessment are recommended if transaminase levels exceed three times the upper limit of normal
- New onset diabetes: some people who take statins are at greater risk of diabetes. It is considered that the risk of statin-induced diabetes is low and outweighed by the potential benefits of reduced CVD risk
- Common side-effects (one in 10) include allergic reactions, headache, nausea, gastro-intestinal disturbances, inflammation of the nasal passages, pain in the throat or nose bleeds.
Statins are contraindicated in pregnancy and in those who are breastfeeding.
Statin intolerance
Statin intolerance is defined as the presence of clinically significant adverse effects from statin therapy that are considered to represent an unacceptable risk to the patient or that may result in adherence to therapy being compromised.
For people who are intolerant of the initial recommended statin, treatment options may include trying a lower dose of the same statin or switching to an alternative statin (in the absence of contraindications; ideally, at least three different statins should be tried).
In some patients, alternate day, or once or twice weekly, dosing strategies may be tolerated (unlicensed) and often this can then be successfully up titrated to the maximum tolerated dose and frequency. More details can be found in the statin intolerance pathway.
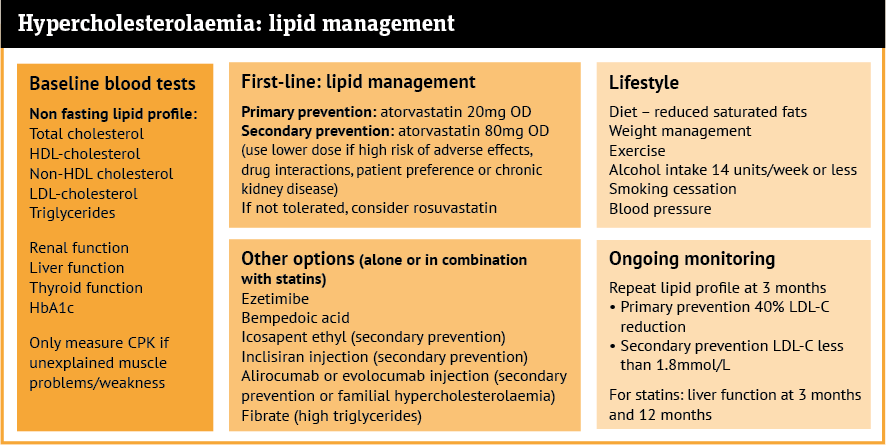
Ongoing monitoring: lipid profile
Two to three months after starting treatment with a statin, a repeat blood test for the lipid profile should be undertaken to assess response to therapy. For those people who do not achieve the required reduction in LDL-C/non-HDL-C, where possible the statin dose should be optimised.
Additional or alternative options should be considered for those people who are unable to tolerate statins at all, or if the maximum or maximum tolerated dose of statin treatment is
not to target.
Alternative or additional lipid lowering approved treatments
Refer to NICE (England, Wales); the Department of Health for Northern Ireland (to check whether NICE guidelines/technology appraisals have been endorsed for use in Northern Ireland); or the Scottish Medicines Consortium for Healthcare Improvement for Scotland as approved place in therapy may differ.
Oral treatment options
Ezetimibe 10mg once a day: This can be used alone or in combination with a statin and will lead to an additional 15-20 per cent reduction in LDL-C. With proven tolerability (main side-effects are gastrointestinal) plus CVD outcome data from the IMPROVE-IT trial, it is often the next option for both primary and secondary prevention.
Bempedoic acid 180mg once a day is a relatively new option – approved for both primary and secondary prevention. It works on the same pathway as statins but does not go into the muscles and as a result, it does not have the muscle side-effects of statins but does increase uric acid levels and therefore may increase the risk of gout. NICE recommends use in combination with ezetimibe in statin intolerant patients. The first outcome trial for bempedoic acid was recently published, providing data to support its use in statin-intolerant patients to reduce CVD events.
Icosapent ethyl, a highly purified form of fish oil, may be added to statin therapy (two capsules twice a day) in selected people where triglycerides are also raised.
Injectable treatment options
Some people may also be prescribed an injectable form of treatment. Inclisiran has been introduced recently for secondary prevention and is administered in a GP surgery (or hospital clinic).
It is possible that a community pharmacy will receive a prescription for the supply of inclisiran for the patient to take to their healthcare provider for administration. Clinical trials are ongoing to better understand its place in treatment pathways.
Specialists may also prescribe a PCSK9 inhibitor (alirocumab or evolocumab), which the patient self-injects. Currently their prescribing and supply remains with secondary care services.
Practice pointer
A patient asks you if she could get the same effect from changing her diet as from taking her medication. How would you respond?