3. Questions to ask during the consultation
These will depend on what has already been established but could run as follows:
“Do you know why you have been prescribed this medicine?”
Tailor the conversation to what you have found out about the indication. This could be primary prevention, secondary prevention or, less commonly, for an inherited lipid disorder such
as familial hypercholesterolaemia (FH).
“Do you have any concerns/questions?”
Many people have heard about statins in the lay media and it is not uncommon for patients to express concerns. They may have family members or friends who are taking a statin. It is important to listen to any concerns but also to remember that, in the large majority of people, the CVD benefits will outweigh the risk of side-effects.
With reference to statins, people should be advised to report any adverse muscle effects promptly to their GP.
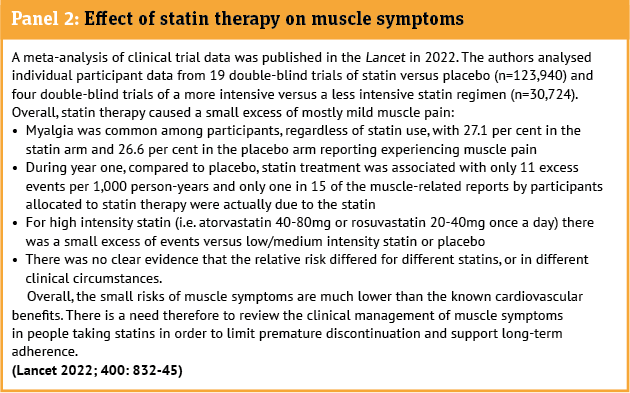
The incidence of adverse muscle effects quoted in the literature can vary quite widely (see panel). This in part depends on whether the data comes from randomised controlled trials (where the numbers are low) or observational studies.
“Does my statin have to be taken at bedtime?”
Both atorvastatin and rosuvastatin can be taken at any time of day. The requirement for the statin to be taken in the evening or at bedtime relates to simvastatin, pravastatin and fluvastatin.
“Have you been given any lifestyle advice?”
Irrespective of a patient’s level of risk, lifestyle modification is considered an integral part of CVD management. Healthy heart advice for hypercholesterolaemia and reducing CVD risk should include, where relevant, healthy eating/diet, exercise, weight management, sensible alcohol intake and smoking cessation. With reference to diet for cholesterol management, Heart UK (heartuk.org.uk) is a useful resource for myth busting and also for recipes.
The degree to which cholesterol is lowered by dietary changes depends on a number of factors such as the quality of the baseline diet, the number and magnitude of dietary changes, and how long these changes are maintained. For some people this may be enough but for others extra help with medication will be needed.
Ketogenic diets (those which severely restrict carbohydrates with a moderate level of protein and no restriction on fats can end up being high in saturated fat and cholesterol and may significantly increase LDL-C levels) are best avoided in general and are contraindicated in people with familial hypercholesterolaemia.
For people at increased CVD risk (e.g. high risk primary prevention, secondary prevention and those with FH), diet should only be seen as an adjunct to statin treatment and as one element in the overall strategy to reduce an individual’s CVD risk.
“What further appointments or follow-up do you have in place?”
After starting a statin a blood test is recommended at two-three months to check the response to treatment in terms of LDL-C/non-HDL-C reduction and to check the liver blood test. If the cholesterol is not treated to target, check adherence to treatment.
Escalation of treatment with a dosage increase or addition of another class of lipid lowering medicine may be required or, in the case of side-effects/intolerance, a change in statin dose and/or class of lipid lowering medicine.
If all is satisfactory a further lipid profile and liver blood test should be undertaken at 12 months.
For other lipid lowering medicines a repeat lipid profile at around three months is also recommended.