1. Pre-consultation
When preparing for a consultation, it is useful to consider the patient’s possible thoughts on taking a medicine for lowering cholesterol. This is especially important if they have been prescribed a statin as there are many pre-conceptions about statin therapy.
This section of the module provides a brief aide mémoire on lipid modification therapy and focuses on statins as the mainstay of therapy.
Lipid modification
The main aim of lipid modification is to reduce low density lipoprotein cholesterol (LDL-C)/non-high density lipoprotein cholesterol (non-HDL-C), which will in turn reduce CVD risk. The NHS has produced a summary of national guidance for lipid management for primary and secondary prevention of cardiovascular disease, which can be used in everyday practice.
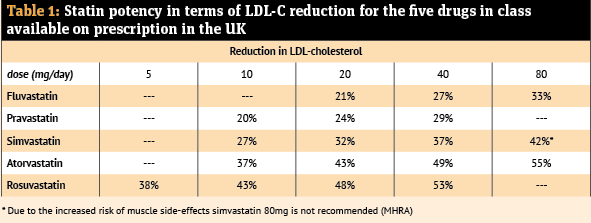
Statins are the first-line therapy for both primary and secondary prevention. Meta-analysis of the numerous large clinical trials concluded that statin therapy results in a 22 per cent relative risk reduction of major cardiovascular events with each 1mmol/L drop in LDL-C. NICE recommends prescribing a statin that will result in a reduction in LDL-C (or non-HDL-C) of at least 40 per cent.
Table 1 details the relative potency of statins. Note that doubling the dose of a statin will lead to a further reduction in LDL-C of a magnitude of 6-7 per cent. While the dose should be titrated to achieve the maximum tolerated, some people may require additional lipid lowering medication to reach their treatment target.
Atorvastatin 20mg once per day is recommended as the first-line option for all primary prevention indications. For secondary prevention, a high-intensity, high-potency statin is the first-line option with atorvastatin 80mg once per day recommended, unless there is a high risk of adverse effects, potential drug interactions, patient preference or chronic kidney disease (then 20mg recommended as the starting dose).
Rosuvastatin offers a cost-effective alternative (with the caveat of a starting dose of 5mg once per day and maximum dosage of 20mg once per day in patients of Asian ethnicity).
An alternative strategy to aiming for a percentage reduction in LDL-C/non-HDL-C is to use target lipid levels – a plan (combined with percentage reductions) used in other international guidelines. Many clinicians prefer target levels, as calculation of percentage reductions can be complex to work out in everyday practice.
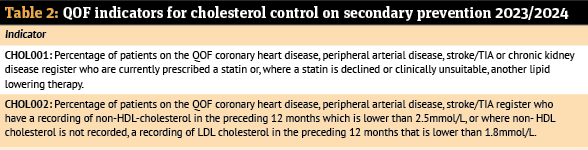
Recognition that in England only 82 per cent of people with established CVD are prescribed statins (or alternative lipid lowering therapy) and that, even if prescribed, less than 30 per cent of people are treated to target has led to the introduction of primary care targets to improve lipid management in patients with established CVD (secondary prevention) or chronic kidney disease with Quality Outcomes Framework (QOF) indicators.
From April 2023, each GP practice in England is eligible to earn up to 30 QOF points (see Table 2) if certain percentage thresholds are met. Community pharmacy is well placed to support and increase patient adherence.
Starting a statin
The decision whether to start statin therapy should be made after an informed discussion between the clinician and patient about the risks and benefits of statin treatment, considering additional factors, such as benefits from lifestyle modification, informed patient preference, comorbidities, polypharmacy, general frailty
and life expectancy.
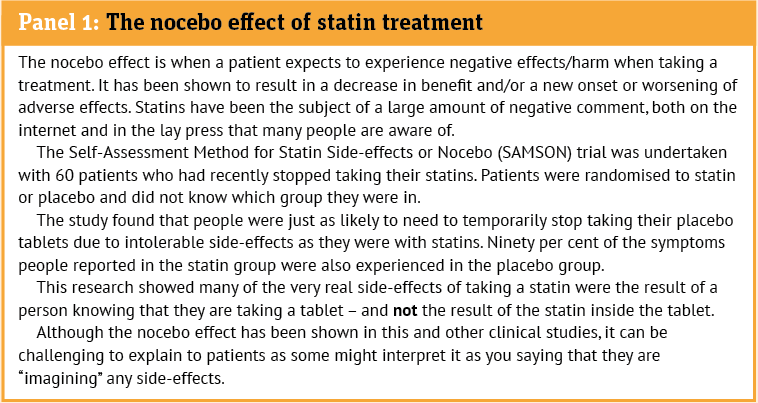
This shared decision-making process is essential as ‘statin reluctance’ (an attitudinal state of aversion to taking statins, often without any prior taking of a statin) and the ‘nocebo effect’ (see panel) can act as barriers to the clinical effectiveness of statin therapy.
In addition to the lipid profile, baseline blood tests should include liver tests, renal function, thyroid function (as hypothyroidism is a secondary cause of hyperlipidaemia and will increase the risk of statin induced myopathy) and HbA1c.
This will help identify any contraindications and rule out any secondary causes of high cholesterol, such as untreated hypothyroidism, nephrotic syndrome, or liver and/or alcohol-related issues.
A baseline creatine kinase (CK) is not required unless the person has generalised unexplained muscle symptoms (e.g. pain, tenderness or weakness), whether associated or not with previous lipid-lowering therapy.
Reflection exercise
A patient tells you he does not really want to take the statin his GP has prescribed. When asked why, he tells you he has friends who had to stop taking them because of side-effects (painful muscles). What three points would you make in response, based on the data about side-effects in studies?