Management of acute attacks
The priority when managing gout is to treat the flare that is the usual presentation: a NSAID (plus proton pump inhibitor if necessary) or colchicine is usually regarded as first-line.
Corticosteroids, whether a short course of an oral preparation or an intra-articular or intramuscular injection, are alternatives, but there are licensing restrictions.
Interleukin-1 (IL-1) inhibitors such as canakinumab are only regarded as options if all else is contraindicated, ineffective or not tolerated, and only then under the supervision of a specialist rheumatology service.
Applying ice packs to the affected joint and resting and elevating the limb can also help alleviate pain, but usually in addition to, rather than instead of, medication.
Acute attacks are painful but self-limiting, usually resolving spontaneously over five to 15 days. As previously mentioned, recurrent acute episodes increase the risk of chronic gout developing with its associated complications – debilitating arthritis, joint damage, renal stones and tophi.
The risk of a repeat episode is 62 per cent in the first year after a first attack, 78 per cent in the second year and 84 per cent in the third year. However, taking preventative action drastically cuts the risk of gout recurrence.
Urate lowering therapy
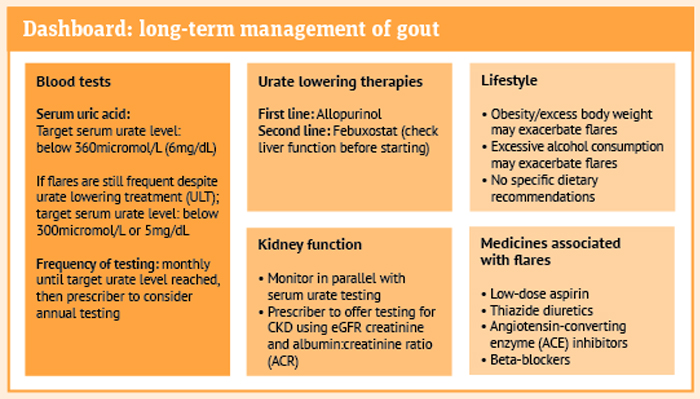
Urate lowering therapy (ULT) should be offered to gout patients who have multiple or troublesome gout attacks, CKD stages 3 to 5, tophi, chronic gouty arthritis or who are on diuretic therapy. A treat-to-target strategy should be adopted, which involves starting with a low dose then increasing it guided by monthly blood tests until reaching the target serum uric acid level of less than 360micromol/L or 6mg/dL.
Patients with tophi or chronic gouty arthritis who continue to experience frequent flares despite having a serum uric acid level at or below this mark may be set a lower target of under 300micromol/L or 5mg/dL.
Allopurinol or febuxostat should be offered as first-line treatments taking into consideration the patient’s comorbidities and preferences. Allopurinol is advised for anyone with major cardiovascular disease such as previous myocardial infarction or stroke, or unstable angina.
The ULT that has not been used can be tried as an alternative if the target serum uric acid level is not reached or side-effects become problematic. Patients should be warned of the risk of a gout exacerbation when starting ULT – ideally at least two weeks should be allowed to elapse after an attack has resolved, but if flares are frequent this may not be possible – and acute medication provided as appropriate.
There is not enough evidence to support any specific diet to prevent gout flares or reduce hyperuricaemia, but a healthy balanced diet is advised. Someone who is overweight or who has excessive alcohol consumption should be advised that these factors increase the risk of acute gout episodes and should address their lifestyle. Any medicines that may be contributing should also be identified and replaced if possible.
Someone on ULT who continues to experience frequent attacks of gout may not be taking their medication as prescribed, perhaps need a dose increase or may have inadvertently triggered an attack due to medication, trauma, diet, weight gain or excessive alcohol consumption.
Staying on track with ULT can be difficult if symptoms are not controlled, so pharmacy teams have a valuable role to play in providing reassurance that continuing treatment will decrease the frequency and intensity of further flares and patients should not stop their treatment.
Referral to a rheumatology service is considered appropriate for patients for whom a diagnosis of gout is uncertain; treatment is contraindicated, not tolerated or ineffective; or who have CKD stages 3b to 5, or have had an organ transplant.
Annual monitoring of serum uric acid levels should be considered for patients on ULT and a watchful eye kept on kidney function, cardio-vascular risk factors and other comorbidities. Liver function tests are needed for individuals on febuxostat.
Patients are likely to benefit from receiving tailored information on gout, including the signs and symptoms; causes and progressive nature of the disease if not managed; risk factors, treatment options for exacerbations; and the long-term nature and benefits of ULT. Signposting to sources of information and support can also be helpful:
Pharmacy teams may find the information published by NICE at nice.org.uk/guidance/ng219 helpful, as well as the Clinical Knowledge Summary.