In Clinical
Follow this topic
Bookmark
Record learning outcomes
Learning objectives
After reading this feature you should be able to:
- Understand the balance of clinical opinion regarding the proposed reclassification of Aquiette (oxybutynin)
- Identify the symptoms, causes and treatment options for overactive bladder
- Advise customers suffering with urinary incontinence on recommended management options.
If the switch to P medicine status is approved, Aquiette would become the first drug for overactive bladder available OTC. Aquiette is indicated for the treatment of long-standing symptoms of overactive bladder in women aged 16-65 years that have persisted for at least one month and which are not adequately controlled by bladder training alone.
Key facts
- The proposed switch of Aquiette would make oxybutynin the first drug available OTC for overactive bladder
- Management options for urinary incontinence and overactive bladder include lifestyle modifications, bladder training, pelvic floor muscle exercises and drug treatments (e.g. antimuscarinics)
- Approximately one in six adults in the UK currently suffer with overactive bladder syndrome
The oxybutynin hydrochloride 2.5mg oral tablet is taken two or three times daily dependent on symptom response. An anticholinergic agent, specifically an antimuscarinic, oxybutynin acts to relieve symptoms of overactive bladder by relaxing the detrusor. This has the effect of increasing the bladder’s capacity to store urine and cutting down on the risk of spontaneous bladder contraction.
“It is vital more medicines are reclassified to pharmacy-only status, enabling people to access them following a short consultation with a pharmacist,” says Anna Maxwell, chief executive of Maxwellia – the UK company behind the proposed POM to P switch of Aquiette.
Dr Julian Spinks, a GP with a specialist interest in the management of incontinence, says an important unmet need currently exists in the treatment of incontinence – one which the OTC availability of Aquiette could help to fill.
The proposal to make low-dose oxybutynin a pharmacy medicine needs to be viewed against a background of the large number of women who suffer from urinary incontinence caused by overactive bladder, he says.
“Despite the increasing visibility of incontin-ence products in adverts, it continues to be a condition which is associated with significant embarrassment and stigma. This can lead to long delays before women seek help from healthcare professionals. These women miss out on early opportunities to treat the underlying cause of their incontinence, such as overactive bladder.”
On the opposing side of the argument is Graham Stretch, chief pharmacist and partner at the Argyle Health Group, president of the Primary Care Pharmacy Association and pharmacy lead of Ealing GP Federation. “Increased use of oxybutynin via the pharmacy route would be unwarranted as the body of evidence increasingly demonstrates both better agents are available and that there is a risk that a cumulative effect from this agent certainly increases dementia risk and may actually cause dementia,” he says.
“We urge the MHRA to refuse this application on grounds of poor safety profile.”
Training programme
The proposed reclassification stipulates that women will be required to try at least six weeks of bladder training before initiating treatment with Aquiette.
Dr Spinks emphasises the importance of the bladder training programme that will be provided alongside Aquiette. “This offers an opportunity for the woman to reduce the progression of her overactive bladder and should diminish the need for ongoing pharmacological treatment at the end of the course.”
Once a patient has completed the required six weeks of bladder training, an initial six-week treatment course of Aquiette may be tried, alongside continuing bladder training and lifestyle measures. If treatment proves successful in controlling symptoms, Aquiette can be continued for a further six weeks – equating to a maximum total treatment course of 12 weeks.
After this, Aquiette must be discontinued and the patient advised to continue with bladder training and lifestyle measures alone. Recurrence of symptoms after three months of treatment should trigger referral to a GP to discuss more suitable longer-term treatment options.
Maxwellia has produced a raft of pharmacy training materials to support the planned switch. These include a pharmacist training guide and a quick reference guide, the latter providing an aide memoire for use during patient consultations to determine if Aquiette is suitable for supply.
The company has also produced a bladder training plan detailing key lifestyle measures and bladder training techniques aimed at improving the symptoms of overactive bladder. The intention is that this will be given to the patients presenting with overactive bladder symptoms and/or requesting Aquiette. The plan includes a checklist on the reverse side for the patient to fill in prior to a consultation with the pharmacist to identify any co-existing conditions that may render Aquiette unsuitable. The patient information leaflet and packaging will reiterate the key safety messages for use of the product.
“The proposed reclassification stipulates that women will be required to try at least six weeks of bladder training before initiating treatment”
PRIME targets pharmacy teams
Researchers at the University of the West of England are calling on pharmacists to participate in the PRIME study (Pharmacy Role in the Promotion of Continence).
PRIME is designed to explore what is feasible to improve bladder and bowel continence closer to home.
Lead researcher Professor Nikki Cotterill says: “We are keen to enable as many voices to be heard from community pharmacy as possible. This really is an opportunity to share your views about the possibilities and difficulties for helping people with bladder and bowel leakage in community pharmacies.”
Weighing up the arguments
One of the key criteria that must be met for pharmacy reclassification of any medicine is that no “direct or indirect danger exists to human health, even when used correctly, if used without medical supervision”. The MHRA, advised by the Commission on Human Medicines, has weighed up this consideration and the three other key reclassification criteria and concluded that: “None apply to Aquiette as all risks can be managed through the product information and pharmacist training.”
Graham Stretch disagrees. “Oxybutynin, even at 2.5mg twice or three times a day for a limited period in the under 65s, is not suitable nor safe for sale without prescription. This is due to mounting evidence implicating association of oxybutynin with cognitive decline, changes in brain architecture – and influential academics are now describing this agent meeting epidemiological (Bradford Hill) tests demonstrating causation of dementia. Oxybutynin also causes acute side-effects of dizziness, confusion, dry mouth, dry eyes, raised intraocular pressure and falls, amongst other adverse effects.”
There is evidence of risk with oxybutynin even used in ‘midlife’ and also as far as 15-20 years before dementia appears, Stretch continues. “The argument that the age limit prevents patients vulnerable to dementia taking the deregulated oxybutynin is false.” He points to several pieces of evidence to support this stance; not least a recent Cochrane review, which concluded that oxybutynin (and other anticholinergic burden [ACB] drugs) “doubles risk of dementia”.
Other studies have reiterated these concerns about an association between cumulative anti- cholinergic use and dementia risk, and suggested potential underlying changes occurring to brain architecture. “The use of medications with anti- cholinergic activity also increased the cumulative risk of cognitive impairment and mortality in a study with 13,000 participants from the UK,” adds Stretch.
On the opposite side of the clinical divide, Julian Spinks argues that the pharmacy-led training and limited duration of Aquiette treatment in the OTC pharmacy setting would succeed in mitigating any risks. “Long-term use of oxybutynin is not suitable for some women, particularly older women who are at a greater risk of physical or mental decline, and NICE recommends it is not used in this group,” he points out.
“However, the current proposal is for short-term [12 weeks maximum], low-dose, oxybutynin in 18 to 65-year-olds. This would only be offered after a pharmacist has assessed to ensure it is appropriate to use in the individual. The dose and duration proposed are highly unlikely to present the same concerns as long-term use of higher-dose anticholinergic medications on prescription.
“An additional proposed protection is that those women who continue to have problems will be advised to seek advice from their doctor.”
Dr Spinks is also keen to highlight the benefits of pharmacy availability of Aquiette that need to be balanced against any potential risk. “Widening the availability of treatment with low-dose oxybutynin to pharmacies offers women with the early stages of overactive bladder an additional way to receive the help they need if they do not wish to consult their GP or a continence service,” he notes.
While Graham Stretch agrees that “over-active bladder is a condition for which better access to medication, after diagnosis and a non-pharmacological treatment trial, would be desirable”, he argues that this should not extend to OTC availability of Aquiette. Of all the anticholinergic medicines, oxybutynin is the worst choice for deregulation, he states.
“Oxybutynin crosses the blood-brain barrier and, for several hours after dosing, impairs cholinergic pathways in the thalamus, striatum, limbic system and neocortex – critically important for memory, learning, attention and other higher brain functions,” he explains.
The MHRA, which has the final say on the matter, says in its consultation document that, “for Aquiette, use is contraindicated in women aged over 65 years of age, maximum daily dosage is low and duration of use is limited to a maximum of 12 weeks, all of which minimise risk of cognitive impairment occurring in women using the product”.
The consultation on the proposed reclassification closed at the end of April and the MHRA is now considering its final decision.
Other types of urinary incontinence
Millions of people in the UK are affected by urinary incontinence and bladder problems, including the estimated one in six adults who are currently suffering with overactive bladder syndrome.
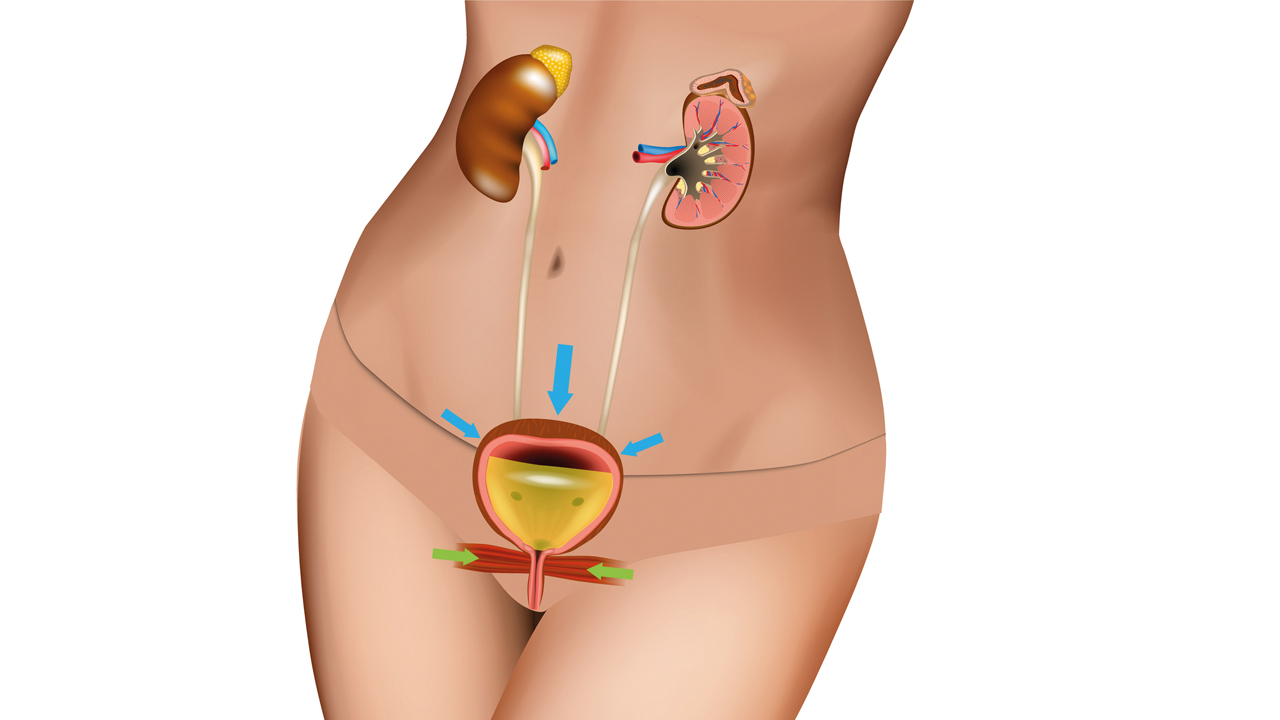
Urinary incontinence that occurs as part of overactive bladder syndrome is known as urge incontinence, where the sudden intense feeling of needing to urinate is followed by the involuntary release of urine.
Other symptoms of overactive bladder include a frequent need to pass urine (more than eight times per day), urinary urgency, the need to urinate at night, urinating during sleep (nocturnal enuresis) and leaking urine during sexual intercourse (coital incontinence).
A cornerstone of treatment for overactive bladder is bladder training. This involves learning techniques and implementing strategies to gradually increase the length of time between feeling the urge to urinate and actually passing urine. Most bladder training courses last a minimum of six weeks and may be accompanied by physical strengthening exercises. These include pelvic floor or kegel exercises that aim to strengthen the detrusor and surrounding muscles.
Dietary modifications can also be implemented to help eliminate known bladder irritants, such as alcohol, caffeine, artificial sweeteners and acidic fruits, but it is important sufferers maintain adequate fluid intake to avoid the urine becoming too concentrated.
Pharmacological options
Pharmacological options for overactive bladder include antimuscarinics, of which oxybutynin, tolterodine and darifenacin are key examples. These drugs work by blocking nerve signals to the bladder that trigger detrusor muscle spasms and contraction, helping to reduce the frequency and severity of the urge to urinate.
Mirabegron is an alternative to anti-muscarinics which also works by promoting detrusor muscle relaxation, thereby allowing the bladder to fill properly and store adequate urine. Other treatment options for more intractable cases of overactive bladder include botox injections into the bladder, nerve stimulation and bladder augmentation surgery.
Aside from overactive bladder, other types of urinary incontinence that may be encountered in the pharmacy setting include stress incontinence – the most common form of bladder weakness – overflow incontinence and mixed incontinence. Pelvic floor muscle training can bring benefits for sufferers of all types of incontinence and works by strengthening the muscles surrounding the bladder and urethra that control the flow of urine during urination.
As adjuncts to a basic pelvic floor muscle training programme, electrical stimulation, biofeedback and/or vaginal cones may be employed. Electrical stimulation is recommended for people who are unable to contract their pelvic flood muscles voluntarily, while biofeedback is a training tool that helps monitor the effectiveness of the exercises being undertaken. Vaginal cones are small weights inserted into the vagina, which are then held in place by the pelvic floor muscles.
Specialist products
Most pharmacies stock specialist, protective incontinence products. These include absorbent pads and pants, bed and chair protection products, and handheld urinals.
The most popular incontinence products are absorbent pads that include a hydrophobic layer to draw urine away from the surface of the pad, thereby keeping the skin dry. In addition to pads, a wide variety of disposal underwear in a range of styles and colours is also now available to purchase.
New developments in products for incontinence include an increased focus on fashion and design, a move to thinner and more breathable products, and an effort to incorporate more sustainable, renewable and bio-based materials.
Smart technologies are also on the horizon, which incorporate a wearable sensor within the product to alert the wearer to the saturation level, helping to facilitate change of pads/pants where required and reduce the risk of leaks.