In Clinical
Let’s get clinical. Follow the links below to find out more about the latest clinical insight in community pharmacy.Follow this topic
Bookmark
Record learning outcomes
Key facts
- More than a quarter of people wait more than a year for a diagnosis of Crohn’s disease or colitis
- For every person diagnosed with coeliac disease, seven to eight remain undiagnosed
- In ulcerative colitis, maintenance therapy with an aminosalicylate is recommended to sustain remission.
Learning objectives
After reading this feature you should be able to:
- Raise awareness and highlight the need for timely diagnosis of lower GI conditions
- Understand the latest thinking in terms of therapeutic interventions
- Recognise how the challenges for patients vary at different stages of life.
Early diagnosis for Crohn’s, ulcerative colitis, coeliac disease and IBD is crucial, as any delay is interruptive to life, limiting people’s capacity to work, participate in education and maintain relationships due to debilitating and worsening symptoms.
Delays to diagnosis also limit treatment options for patients and make hospital admission or surgery more likely.
More than a quarter of people wait more than a year for a diagnosis of Crohn’s or colitis, both of which are inflammatory bowel diseases. During this time debilitating symptoms like severe stomach pain and diarrhoea mean that up to half of patients will end up in A&E while waiting for a diagnosis.
A significant amount of stigma and mis-understanding surround these conditions, so people may suffer in silence unaware that they have an inflammatory bowel condition. They may think that symptoms such as abdominal pain, diarrhoea and unintended weight loss are not serious enough or they may feel scared or embarrassed and not be able to find the right words to describe how they feel.
These issues are particularly significant in younger people aged 18-35 years where one in five lack the confidence to describe their symptoms and one in six feel embarrassed. Lack of knowledge of symptoms for these conditions is also a factor. Three in five young adults do not know that diarrhoea, abdominal pain and blood in faeces are key symptoms of Crohn’s and colitis.
Diarrhoea and abdominal pain are commonly presenting symptoms in pharmacy. While many cases of diarrhoea are short-lived and likely due to food or another source or infection, it is important to check the severity and duration of the symptoms, whether there has been any change in the colour of the faeces indicating blood (e.g. black or bright red), whether diarrhoea alternates with constipation and if the patient is experiencing any abdominal pain or has unintentionally lost weight.
Any or all of these symptoms require further investigation and referral to a GP. Adopting a simple straightforward process to identify these red flag-type symptoms is more important than trying to identify whether the person has an inflammatory bowel condition and which one it might be. There is significant overlap in the symptoms of lower GI conditions which makes diagnosis challenging without further tests.
The key thing is for pharmacy teams to facilitate the patient getting to their GP quickly to start the diagnostic process. Advise the patient to be clear about symptoms and not to be embarrassed. Suggest wording to use and encourage them to write things down before the appointment. It is important to include a full description of symptoms, when they come and go, how often they occur and how long they have had them.
If a diagnosis of a lower GI condition is made, coming to terms with it can be hard. Such conditions impact all aspects of life, including work and personal and sexual relationships. Patients need expert care from specialist doctors, nurses, dietitians, pharmacists and psychologists.
Support from friends, family, colleagues and community pharmacy teams is also important. Many children with IBD worry they will no longer be able to eat with friends and enjoy their favourite foods – but because of compromised nutrient absorption it is vital for children to eat a healthy diet. Among older people with these conditions, diarrhoea can cause dehydration. Fluid intake is vital, as is adherence to medication.
Bowel cancer campaign
Bowel cancer is the third most common cancer in men and women and needs to be diagnosed quickly to ensure the best possible treatment outcomes.
Bowel Cancer UK has launched a new campaign (see bowelcanceruk.org.uk/campaigning/tell-your-gp-instead). Tell Your GP Instead is aimed at people who are likely to delay, often as long as six months, before seeing their GP – even when they have red flag symptoms.
Pharmacy teams should watch out for anyone describing any of the symptoms of possible bowel cancer, such as a change in toilet habits (going less frequently, diarrhoea or constipation that might come and go) and asking for medication for these symptoms.
It is important to ask questions about any blood on toilet paper, a change in colour of the faeces (particularly if they are black and tarry), losing weight unintentionally, feeling tired without knowing why or a pain or lump in the stomach.
Young people should not be overlooked as there are 2,600 cases diagnosed in this age group each year.
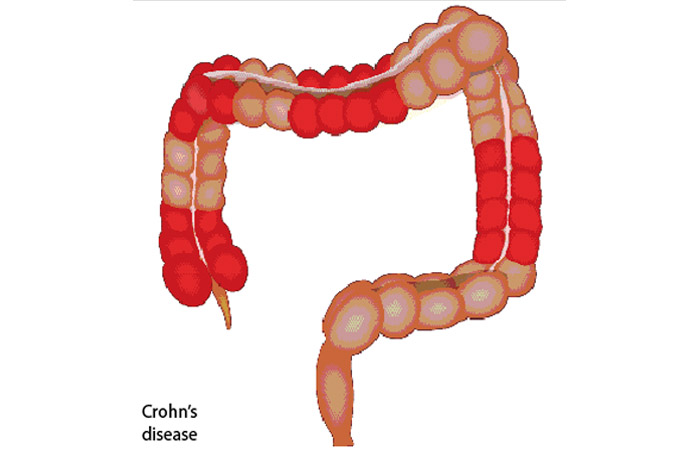
Crohn’s disease
Crohn’s disease is an autoimmune condition where the immune system starts to attack the gut. This causes inflammation and ulcers anywhere in the gut although it most commonly occurs in the small intestine and colon. Symptoms can include pain, diarrhoea, tiredness and blood in the faeces, but other parts of the body can become inflamed (e.g. eyes, joints or skin). Fatigue, feeling generally unwell, anaemia and loss of appetite are common.
Weight loss occurs due to diarrhoea and poor absorption of nutrients. The diarrhoea can be severe enough to prevent the patient getting to the loo in time. Crohn’s is a lifelong condition and varies through periods of remission where symptoms are largely under control and flare-ups where symptoms are more active.
Treatment is directed at the induction and maintenance of symptom remission. A corticosteroid (e.g. prednisolone, methyl-prednisolone) is used to induce remission or treat a single flare-up in a 12-month period. Azathioprine, mercaptopurine or budesonide can be used as add-on therapy to induce remission, and azathioprine or mercaptopurine to maintain remission. Loperamide or codeine phosphate can be used to treat diarrhoea in those who do not have colitis. Colestyramine is also licensed for diarrhoea in Crohn’s.
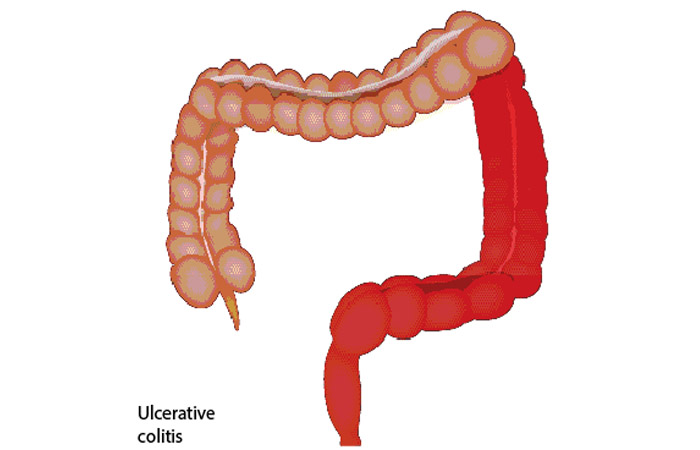
Ulcerative colitis
Similarly to Crohn’s disease, ulcerative colitis is an autoimmune condition where the immune system starts to attack the gut but, unlike Crohn’s, ulcerative colitis causes ulcers and inflammation in the colon and rectum only. Symptoms across the two conditions are similar – diarrhoea, cramping pain, need to get to the loo very quickly, blood in the faeces, loss of appetite and weight, anaemia and tiredness.
Symptoms may vary slightly depending on the type of colitis: proctitis is where only the rectum is affected; left side (distal) colitis is where pain is felt on the left side. Total colitis is where pain can be severe throughout the abdomen. Tenesmus, where there is an urge to go to the loo with an empty bowel, is common to all types of colitis.
Like Crohn’s, ulcerative colitis is a lifelong condition, although most people experience times when the condition is largely in remission and flare-ups when symptoms are active. Although ulcerative colitis is a bowel condition, having an overactive immune system and ongoing inflammation can also lead to inflammation in
the joints, eyes or skin.
Management is focused on treating active disease and symptoms while inducing and maintaining remission. Clinical severity and extent of the disease are important factors. A topical aminosalicylate is most commonly used and an oral aminosalicylate if remission is not achieved. An oral corticosteroid should be considered in patients for whom aminosalicylates are not suitable.
Maintenance therapy with an aminosalicylate is recommended to maintain remission. There is no evidence to support the use of methotrexate to induce or maintain remission although it is commonly used in practice.
New treatments for IBD
A range of biologic drugs (e.g. adalimumab, infliximab), Janus kinase inhibitors (e.g. filgotinib) and sphingosine-1-phosphate (S1P) receptor modulators (e.g. ozanimod) are used for maintaining remission of IBD. Others are in the pipeline:
- Etrasimod is an oral S1P receptor modulator, which adheres to a protein on white blood cells stopping them travelling to the gut where they cause inflammation. It is being assessed for the treatment of Crohn’s disease
- Guselkumab is an injectable biologic medicine that works by blocking interleukin (IL)-23, a protein naturally produced in the gut that fights infection but can result in inflammation. NICE is assessing this drug for people who cannot take or have not responded to standard treatments for moderate to severe ulcerative colitis and Crohn’s disease
- Mirikizumab is a biologic that has been accepted by NICE for treatment of colitis and is being assessed for Crohn’s
- Rizankizumab is a biologic accepted by NICE for treating Crohn’s and is being assessed for colitis.
New drug targets for IBD are emerging, including a cellular protein PAK-2 and an immune protein IL-17. A UK research team recently identified a weak spot in the DNA of 95 per cent of patients with IBD, which makes it easier for some immune cells to drive inflammation in the gut. This section of DNA appears to be the main regulator for macrophages and cytokine release, producing inflammation. The researchers found that some people are born with a fault in this part of the genetic code that leads to a huge inflammatory response. Clinical trials could start in the next five years.
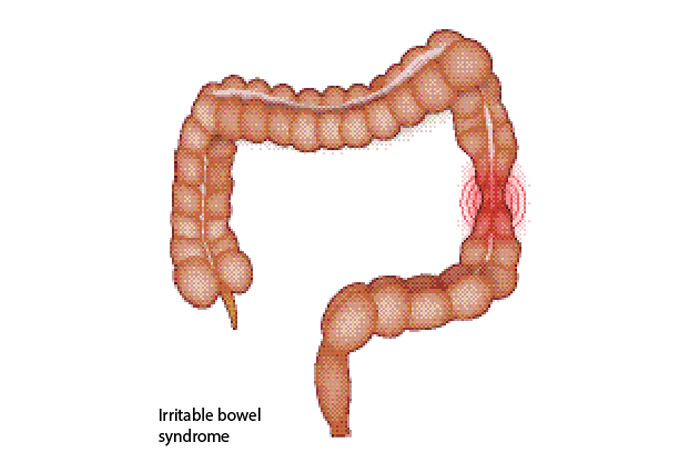
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a different condition to Crohn’s or colitis, albeit with some similar symptoms. The condition can cause abdominal pain or cramps, but these are often worse after eating and better after passing a motion. IBS also causes bloating, diarrhoea, flatulence, tiredness, nausea, constipation, faecal incontinence, backache and the need to pass urine urgently and frequently. It is more common than irritable bowel disease.
Both Crohn’s and colitis cause inflammation in the bowel and blood in faeces – but IBS does not. Some people with colitis also develop IBS symptoms, and have pain and diarrhoea even when the colitis is not active. IBS is a lifelong condition in which symptoms come and go over weeks and months.
IBS is often triggered or made worse by stress and anxiety. Many IBS sufferers also suffer from anxiety and depression. Understanding how the symptoms affect the patient’s life and providing support to try dietary and lifestyle modifications are key to helping sufferers.
Careful discussion with the patient to exclude more serious conditions is essential. IBS can be managed in pharmacy but only when it has been diagnosed by a GP.
Refer patients to the GP when there is:
- Persistent constipation (with concomitant weight gain, lethargy, cold intolerance, fatigue, non-specific weakness, aches and pains which could indicate hypothyroidism)
- Persistent diarrhoea (could indicate coeliac disease, inflammatory bowel disease or gastroenteritis)
- Blood in the stools or bleeding, symptoms suggestive of bowel obstruction (vomiting, colicky pain, abdominal distension) or persistent change in bowel habit (i.e. over two weeks or longer) differing from a pattern of going to the toilet over months and years.
Children, pregnant women and patients unresponsive to lifestyle and OTC treatments should also be referred, as should people with any new symptoms.
Diet can help but no one diet suits all patients. The NICE guideline on IBS recommends having a healthy diet with regular meals, adequate fluid intake, limiting high fibre foods such as wheat bran and limiting caffeine. Avoiding sorbitol (found in many food products and diet drinks) can help.
Food intolerances (e.g. dairy, onion, leeks, garlic, fructose) have been implicated in triggering symptoms in some patients. Probiotics can help some patients and advice can be given to try a course for four weeks to see if it makes a difference.
Radical dietary restrictions, including the low FODMAP (short chain carbohydrates that are not fully absorbed in the gut) diet, should not be tried without a dietitian’s guidance as the patient can risk nutrient shortfalls.
Patients should reduce stress as much as possible with regular exercise to contribute to overall well-being.
Various OTC medicines can also help relieve symptoms and improve quality of life.
- Bulk forming laxatives (sterculia, ispaghula) rather than stimulant or osmotic laxatives (as they may aggravate the condition) can help for constipation. Oat bran is also worth a try as it is a soluble fibre and likely to be less of an irritant than wheat bran. Remind the patient to take on more fluids when increasing fibre
- Loperamide for diarrhoea (OTC use in IBS is restricted to patients aged 18 or over and when
a diagnosis of IBS has been made by a doctor) - Antispasmodics are available OTC and may be helpful for patients suffering from abdominal pain. Smooth muscle relaxants alverine, mebeverine and peppermint oil and the antimuscarinic hyoscine are used. Side-effects from the smooth muscle relaxants are rare, but hyoscine may cause anticholinergic side-effects (e.g. dry mouth, blurred vision). Efficacy does not vary between antispasmodics but patients often respond better to one than another.
Check dosing and licence restrictions before recommending. Alverine and mebeverine should not be used in children and pregnant women. Peppermint oil should not be used in children. Hyoscine can be used in adults and children over six years (not all brands).
Symptom improvement should occur within a few days so ask the patient to return to the pharmacy after a week to monitor progress. It is worth trying another antispasmodic if the first one has not worked. Patients may need to try several treatments until they find one that suits them. Check what medication the patient has tried and whether it has produced improvement.
“The important thing is for pharmacy teams to facilitate the patient getting to the GP quickly to start the diagnostic process”
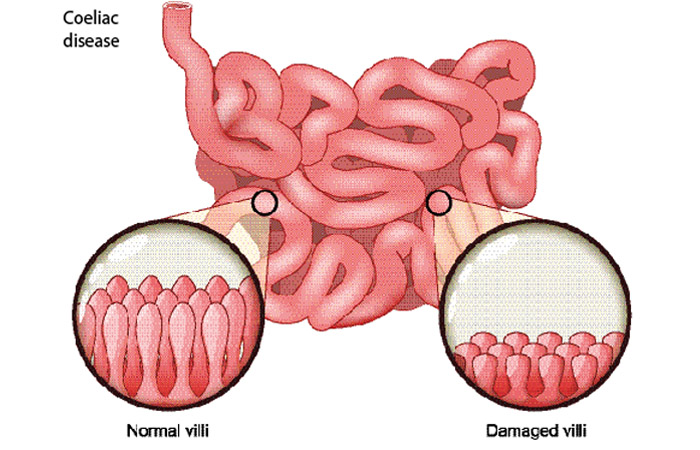
Coeliac disease
Coeliac disease is an autoimmune condition driven by immune responses to gluten, which leads to damage of the villi in the lining of the small intestine. Gluten is a complex protein found in wheat, rye, barley, wheatberries, emmer, einkorn, semolina and spelt.
Coeliac disease is characterised and diagnosed by the presence of coeliac-specific autoantibodies and a range of gastrointestinal symptoms of varying severity. Gluten intolerance (or non-coeliac gluten sensitivity) describes an intolerance to gluten with symptoms similar to those of coeliac disease, yet a lack of the same antibodies and intestinal damage as seen in coeliac disease.
Symptoms include diarrhoea with malabsorption causing high levels of fat in the stools (steatorrhoea). Other symptoms include abdominal pain, bloating and flatulence, indigestion, constipation, and vomiting (mainly in children). More general symptoms include fatigue (which may be due to deficiency of iron or vitamin B12), unexpected weight loss, inability to conceive, peripheral neuropathy, oedema of the hands, feet, arms and legs, and disorders affecting co-ordination, balance and speech (ataxia).
Pharmacists should consider the presentation of such symptoms carefully and refer where necessary. An autoimmune reaction to gluten can lead to dermatitis herpetiformis, an itchy skin rash (most commonly on the knees, elbows and buttocks) with blisters that burst when scratched. It occurs in around 20 per cent of people with coeliac disease.
The prevalence of coeliac disease (using serological testing and including previously diagnosed patients) is about 1 per cent in the UK. However, coeliac disease is under-diagnosed. It is estimated that for every person diagnosed, seven to eight remain undiagnosed. The prevalence has increased over the past 50 years (possibly due to improved identification and diagnosis). Coeliac disease affects all age groups, including older people, with 70 per cent of new cases diagnosed in people over the age of 20 years.
The only effective management for coeliac disease is long-term adherence to a gluten-free diet. This can be a difficult for patients to follow and children will need extensive support. Referral to a dietitian can help to educate the patient and check for any nutritional deficiencies (e.g. vitamin B12, vitamin D, iron and calcium).
Pharmacy teams can support patients with their prescriptions for gluten-free products ensuring availability of stocks with as much choice as possible. Dietary advice is essential so that gluten-containing foods are avoided.
Resources for lower GI problems
- Crohn’s and Colitis UK is a national charity that provides support for people of all ages with ulcerative colitis and their families. crohnsandcolitis.org.uk
- The Crohn’s and Colitis Foundation focuses on improving the quality of life for people with these conditions:
crohnscolitisfoundation.org - NICE Guidelines for Diagnosing and Managing Inflammatory Bowel Disease in Adults and Children. nice.org.uk/guidance/qs81
- Crohn's disease: management. National Institute for Health and Care Excellence. Clinical guideline 129. May 2019: nice.org.uk/guidance/ng129
- Ulcerative colitis: management:
nice.org.uk/guidance/NG130 - NICE Guideline for Diagnosis and Management of IBS in Adults:
nice.org.uk/guidance/cg61 - The Coeliac UK website (coeliac.org.uk) contains information on gluten-free food groups, labelling and an updated list of safe foods and drinks, recipes and availability of gluten-free foods on prescription.